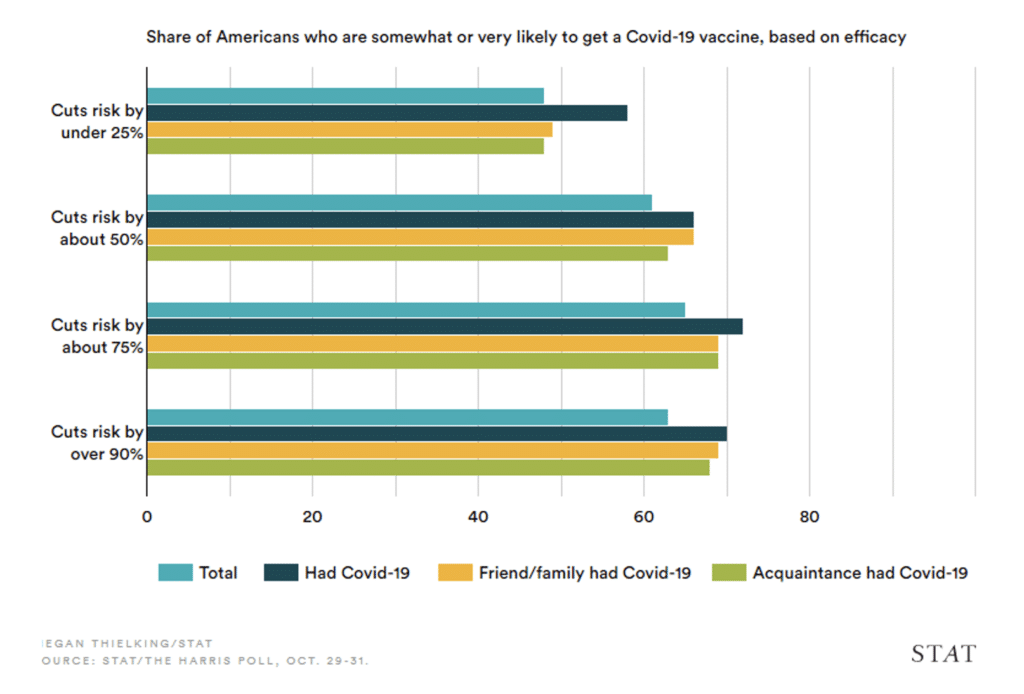
The world is racing to develop a vaccine against COVID-19, something that many believe will put their fears around this virus to rest. The latest Gallup and STAT-Harris polls suggest that at least half of Americans would get the vaccine if it were provided free of charge, even if it only cut risk by under 25% [1,2].
It’s understandable that most Americans are willing to get a vaccine. They’re scared, and they want to protect themselves and their family from COVID. What doesn’t make sense is that many of these same Americans are vitamin D deficient or insufficient.
According to the Endocrine Society, a vitamin D status of less than 20 ng/mL (50 nmol/L) is considered a deficiency, 20–30 ng/mL (50–75 nmol/L) is an insufficiency, and more than 30 ng/mL (75 nmol/L) is compatible with optimal health and considered sufficient [3].
These recommendations line up well with the vitamin D concentrations of indigenous tribes in Africa: 25–68 ng/mL (60–170 nmol/L), with an average of ~45 ng/mL (110 nmol/L) [4,5]. It’s likely these were the levels we evolved with and under which our immune system developed.
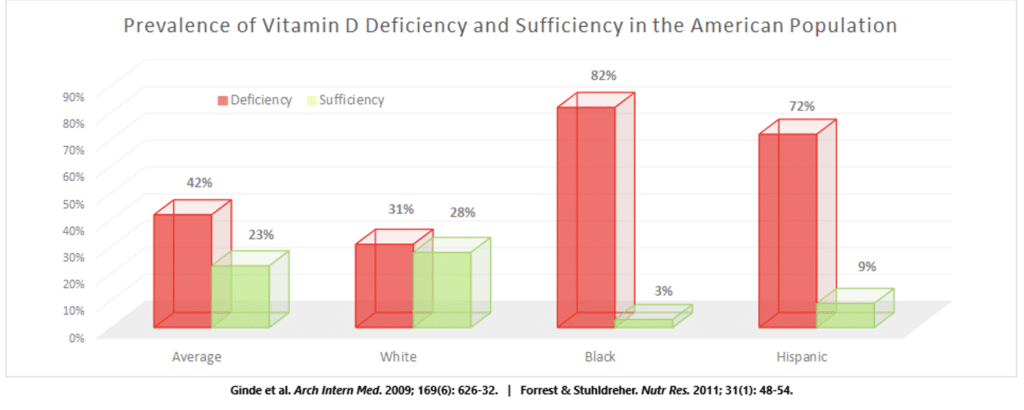
Yet, 42% of Americans are vitamin D deficient, including 80% of the Black population and 63% of the Hispanic population [6]. When we take into account vitamin D insufficiency, only 23% of the American population has sufficient vitamin D levels, including only 5% of Black Americans and 10% of Mexican Americans [7].
While not really surprising considering that we transitioned from a “people of the sun” to a “people of the cubicle”, it is disheartening considering the essential role of vitamin D in protecting us from infectious diseases.
In fact, I’d wager that if a simple vitamin D supplement were a vaccine, it’d be considered a miraculous breakthrough in COVID prevention and treatment. My goal with this article is to show you why.
How Vitamin D Fights Infections
Vitamin D fights infections in two fundamental ways: it enhances our immune defenses and bolsters the resilience of our tissues and organs. This means that vitamin D can help prevent us from becoming infected altogether, as well as reduce the severity of any infection that does take hold.
For example, every immune cell in our body has vitamin D receptors and responds to its signal, with the overarching effects being to suppress inflammation, promote immune tolerance, and maintain proper functionality of immune cells [8,9]. A great example of its importance is T-cells.
T-cells are a critically important aspect of our adaptive immune system. They are the cells that communicate with all other immune cells to coordinate attacks against invaders, as well as develop into a special type of cell that functions to eliminate very specific targets with minimal tissue damage, such as cancer cells or cells infected with viruses.
In the case of COVID, several studies have found that a more potent T-cell response reduces the severity of the infection — there are more asymptomatic or mild cases [10–12]. And guess what T-cells require in order to mobilize? Vitamin D! Adequate vitamin D is critically important for the activation of T-cells from their inactive state [13].
As another example, consider the antimicrobial peptide cathelicidin, which is produced by innate immune cells and respiratory epithelial cells in response to infection by bacteria, viruses, and fungi [14]. It functions to both directly kill invading pathogens and also neutralize any endotoxins they might release [15]. Yet, this powerfully protective compound requires vitamin D to be produced [16,17].
Lastly, high levels of vitamin D are critical for first line immune defences including physical mucosal defences, tight junctions, gap junctions, and adherens junctions [18,19], all of which are disturbed by viral and bacterial infections as part of their efforts to establish a stronghold within the body [20,21].
Without adequate vitamin D circulating through the body, our innate and adaptive immune defenses are sabotaged against bacterial and viral assaults [22,23].
Quite simply, vitamin D deficiency predisposes us to infections.
What Does Clinical Evidence Say?
So, the biological plausibility is there — the mechanistic rationale for vitamin D in preventing and treating infections doesn’t just exist, it’s incredibly strong. But even so, theory must take a backseat to experimental investigations.
As the renowned physicist Richard Feynman once said, “It doesn’t matter how beautiful your theory is, it doesn’t matter how smart you are. If it doesn’t agree with experiment, it’s wrong.”
Thankfully, there have been numerous investigations looking at the effect of vitamin D supplementation on the risk of experiencing respiratory tract infections. The most recent, largest, and well-conducted meta-analysis pooled data from 25 randomized controlled trials with nearly 11,000 participants from 15 different countries on four continents [24,25].
Vitamin D supplementation was found to reduce the risk of acute respiratory infection by 12% — only 33 individuals would require supplemental vitamin D to prevent just 1 of them from suffering a respiratory infection.
The benefits were most pronounced with daily or weekly dosing, as opposed to taking huge monthly boluses that weren’t significantly protective. When using this smaller and more frequent dosing regimen, supplementation reduced the risk of respiratory infections by 25–75% depending on how deficient a person was.
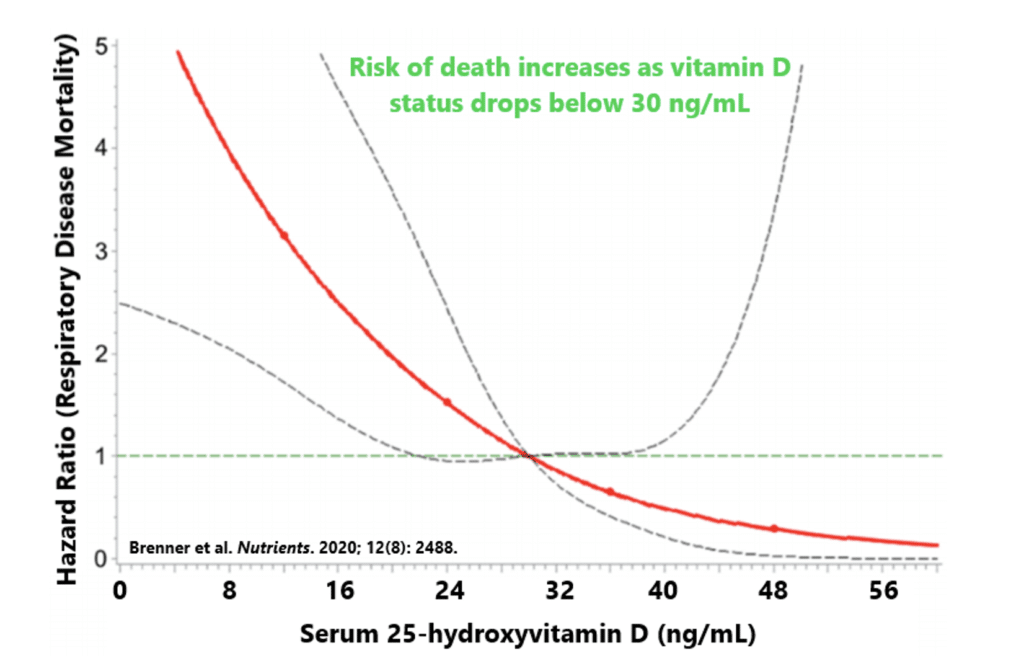
If you do happen to become infected, vitamin D can help prevent more severe complications. For example, one study followed over 9,500 older adults for 15 years and found that the risk of dying from respiratory infections increased substantially as vitamin D status dropped below 30 ng/mL (75 nmol/L) [26]. Just having a vitamin D status of 20 ng/mL (50 nmol/L) doubled the risk of death compared to 30 ng/mL (75 nmol/L).
These observations are largely upheld when it comes to COVID specifically. As you’re about to see, the totality of evidence supports obtaining sufficient vitamin D status as a means of preventing and reducing the severity of COVID-19 [27].
Vitamin D Reduces COVID Severity
First and foremost, we all become sick every now and again. No matter the illness, the goal is to make it as bearable and harmless as possible. Vitamin D can help make that a reality.
Published online in June, 2020, researchers from France, Canada, and China determined that vitamin D status is a biological determinant of COVID outcomes using the Bradford Hill criteria for causality [28].
This criteria is used when there is a lack of interventions for determining whether a causal relationship exists between two variables. This can be incredibly helpful when it would be unethical to expose people to certain variables like cigarette smoke, which is where the Bradford Hill criteria made its debut — showing that smoking causes lung cancer.
Basically, since it would be unethical to expose people to COVID-19, the researchers used the available mechanistic and observational evidence to show that a causal link is likely between vitamin D status and COVID outcomes, whereby deficiency increased the susceptibility to infection and the severity of infectious outcomes.
For example, adults admitted to Spanish hospitals for COVID had better lung function, lower medication requirements, lower ICU admissions, and a shorter hospital stay if their vitamin D status was above 20 ng/mL (50 nmol/L) [29].
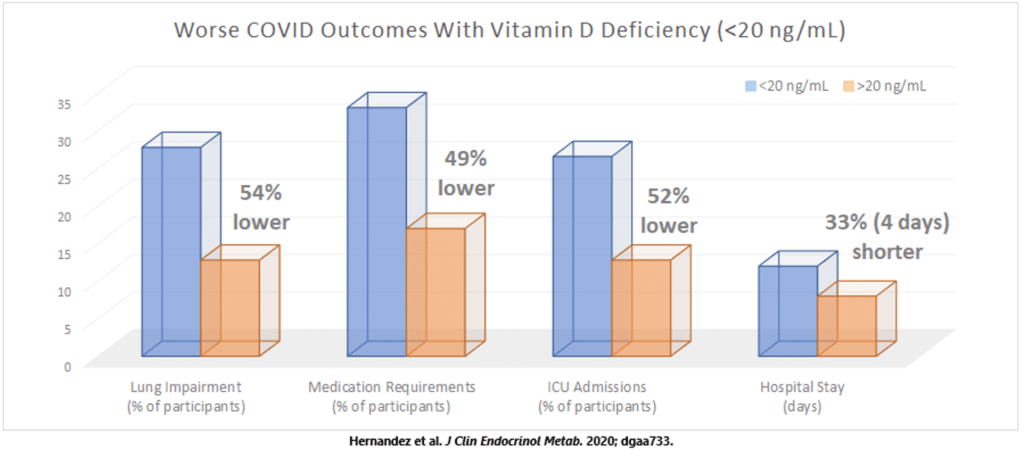
In other studies, vitamin D deficiency was associated with a 2–3-fold greater risk of having more severe COVID outcomes and a 6-fold greater risk of requiring invasive mechanical ventilation or death, even after adjusting for age, sex, and the presence of comorbidities [30–34].
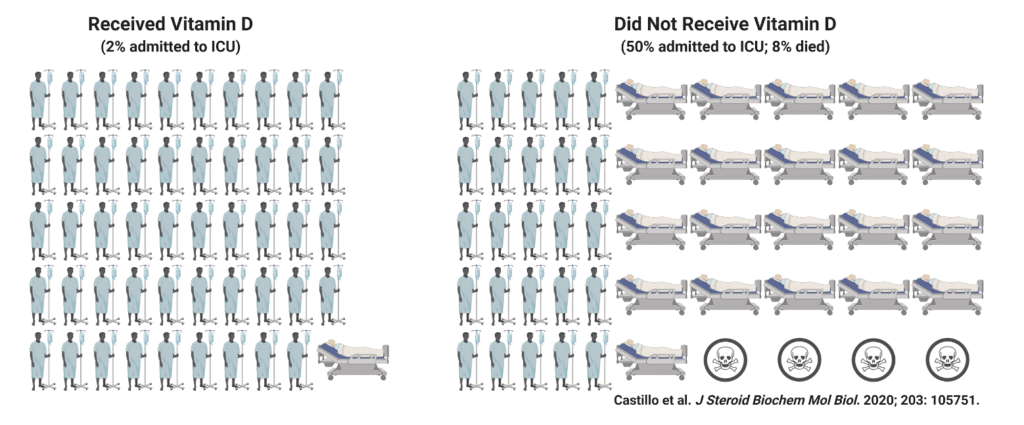
Two months after the Bradford Hill criteria were satisfied for vitamin D and COVID, supportive experimental evidence finally emerged. It was a relatively simple study in which researchers from Spain randomly allocated adults showing up to their hospital with a COVID infection to receive standard medical care with or without supplemental vitamin D [35].
Of the 50 adults who were given vitamin D, only one (5%) required admission to the intensive care unit (ICU), compared to 13 of the 26 adults (50%) who didn’t receive vitamin D. In other words, simply adding vitamin D to the standard of care for COVID reduced the odds of requiring ICU admission by 97%!
These findings make sense. COVID-19 is a respiratory virus that infiltrates cells of the lungs and causes an exacerbated inflammatory response, leading to impaired breathing ability and severe pneumonia [36,37]. This is what can kill you in a severe infection.
However, this intense inflammatory response, also called a cytokine storm, is likely inhibited by vitamin D [38], a conclusion supported by previous research in rodents showing that vitamin D reduces markers of both lung inflammation and lung damage following drug-induced injury [39,40].
All-in-all, one of the best things you can do for your health is ensure an adequate vitamin D status. If you happen to catch COVID while your vitamin D is low, then it’s probably a good idea to start supplementing right away.
Vitamin D Protects Against COVID Infections
What’s cool about ensuring optimal vitamin D levels year-round is that it will likely reduce the risk of catching COVID to begin with, which makes all the previous information somewhat moot.
For example, a study of over 190,000 adults living in all 50 US states found a clear inverse relationship between COVID prevalence and vitamin D status, with a plateau occurring at around 55 ng/mL (135 nmol/L) [41]. Roughly every 1 ng/mL (2.5 nmol/L) increase in vitamin D status was associated with a 2% reduction in the likelihood of being infected.
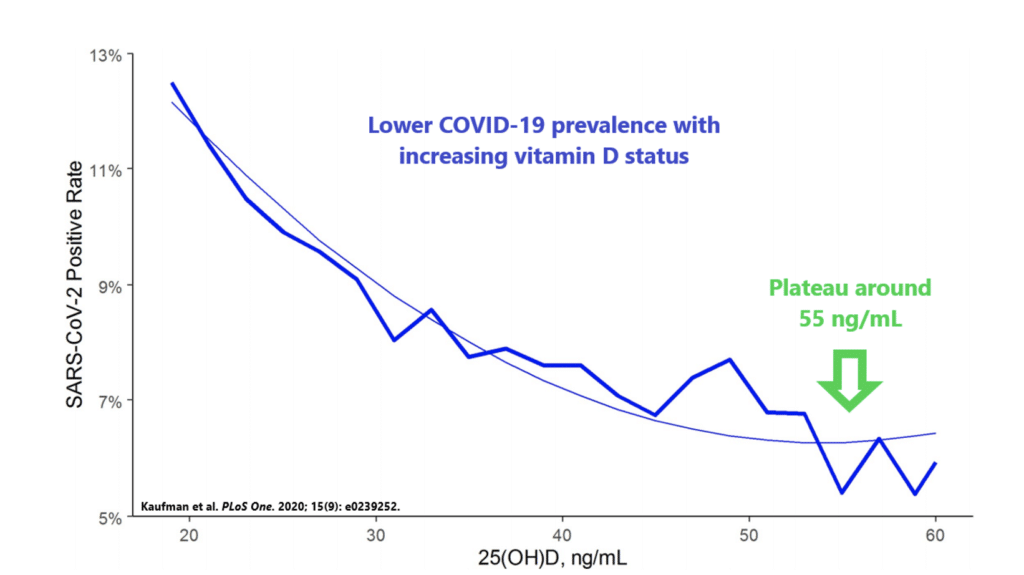
Other smaller studies have confirmed this association, whereby people who test positive for COVID-19 tend to have lower vitamin D levels, on average [42,43]. Interestingly enough, a study of 34 countries on every continent found that COVID-19 cases are more common in areas of the world where there is less UVB exposure [44], which is necessary for vitamin D production in the skin.
Vitamin D is a Vaccine Against COVID-19
This isn’t to say those things aren’t important, only that vitamin D supplementation and regular sun exposure should be on the list with them.
References
- Silverman E, Facher L, Garde D, Feuerstein A, Herper M, Florko N. STAT-Harris Poll: Most won’t get a Covid-19 vaccine unless it halves risk [Internet]. 2020 [cited 2020 Nov 14]. Available from: https://www.statnews.com/pharmalot/2020/11/10/harris-poll-covid19-vaccine-masks-distancing/
- Saad L. Americans’ Readiness to Get COVID-19 Vaccine Falls to 50% [Internet]. Gallup. 2020 [cited 2020 Nov 14]. Available from: https://news.gallup.com/poll/321839/readiness-covid-vaccine-falls-past-month.aspx
- Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911–30. Available from: https://pubmed.ncbi.nlm.nih.gov/21646368/
- Luxwolda MF, Kuipers RS, Kema IP, Dijck-Brouwer DAJ, Muskiet FAJ. Traditionally living populations in East Africa have a mean serum 25-hydroxyvitamin D concentration of 115 nmol/l. Br J Nutr. 2012;108:1557–61. Available from: https://pubmed.ncbi.nlm.nih.gov/22264449/
- Luxwolda MF, Kuipers RS, Kema IP, van der Veer E, Dijck-Brouwer DAJ, Muskiet FAJ. Vitamin D status indicators in indigenous populations in East Africa. Eur J Nutr. 2013;52:1115–25. Available from: https://pubmed.ncbi.nlm.nih.gov/22878781/
- Forrest KYZ, Stuhldreher WL. Prevalence and correlates of vitamin D deficiency in US adults. Nutr Res. 2011;31:48–54. Available from: https://pubmed.ncbi.nlm.nih.gov/21310306/
- Ginde AA, Liu MC, Camargo CA Jr. Demographic differences and trends of vitamin D insufficiency in the US population, 1988-2004. Arch Intern Med. 2009;169:626–32. Available from: https://pubmed.ncbi.nlm.nih.gov/19307527/
- Vanherwegen A-S, Gysemans C, Mathieu C. Regulation of Immune Function by Vitamin D and Its Use in Diseases of Immunity. Endocrinol Metab Clin North Am. 2017;46:1061–94. Available from: https://pubmed.ncbi.nlm.nih.gov/29080635/
- Chun RF, Liu PT, Modlin RL, Adams JS, Hewison M. Impact of vitamin D on immune function: lessons learned from genome-wide analysis. Front Physiol. 2014;5:151. Available from: https://pubmed.ncbi.nlm.nih.gov/24795646/
- Doshi P. Covid-19: Do many people have pre-existing immunity? BMJ. 2020;370:m3563. Available from: https://www.bmj.com/content/370/bmj.m3563
- Chen Z, John Wherry E. T cell responses in patients with COVID-19. Nat Rev Immunol. 2020;20:529–36. Available from: https://www.nature.com/articles/s41577-020-0402-6
- Wang Z, Yang X, Zhou Y, Sun J, Liu X, Zhang J, et al. COVID-19 Severity Correlates with Weaker T-Cell Immunity, Hypercytokinemia, and Lung Epithelium Injury. Am J Respir Crit Care Med. 2020;202:606–10. Available from: https://www.atsjournals.org/doi/full/10.1164/rccm.202005-1701LE
- von Essen MR, Kongsbak M, Schjerling P, Olgaard K, Odum N, Geisler C. Vitamin D controls T cell antigen receptor signaling and activation of human T cells. Nat Immunol. 2010;11:344–9. Available from: https://pubmed.ncbi.nlm.nih.gov/20208539/
- Herr C, Shaykhiev R, Bals R. The role of cathelicidin and defensins in pulmonary inflammatory diseases. Expert Opin Biol Ther. 2007;7:1449–61. Available from: https://pubmed.ncbi.nlm.nih.gov/17727333/
- Dürr UHN, Sudheendra US, Ramamoorthy A. LL-37, the only human member of the cathelicidin family of antimicrobial peptides. Biochim Biophys Acta. 2006;1758:1408–25. Available from: https://pubmed.ncbi.nlm.nih.gov/16716248/
- Liu PT, Stenger S, Li H, Wenzel L, Tan BH, Krutzik SR, et al. Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response. Science. 2006;311:1770–3. Available from: https://pubmed.ncbi.nlm.nih.gov/16497887/
- Gombart AF. The vitamin D-antimicrobial peptide pathway and its role in protection against infection. Future Microbiol. 2009;4:1151–65. Available from: https://pubmed.ncbi.nlm.nih.gov/19895218/
- Schwalfenberg GK. A review of the critical role of vitamin D in the functioning of the immune system and the clinical implications of vitamin D deficiency. Mol Nutr Food Res. 2011;55:96–108. Available from: https://pubmed.ncbi.nlm.nih.gov/20824663/
- Shi Y-Y, Liu T-J, Fu J-H, Xu W, Wu L-L, Hou A-N, et al. Vitamin D/VDR signaling attenuates lipopolysaccharide‑induced acute lung injury by maintaining the integrity of the pulmonary epithelial barrier. Mol Med Rep. 2016;13:1186–94. Available from: https://pubmed.ncbi.nlm.nih.gov/26675943/
- Rossi GA, Fanous H, Colin AA. Viral strategies predisposing to respiratory bacterial superinfections. Pediatr Pulmonol. 2020;55:1061–73. Available from: https://pubmed.ncbi.nlm.nih.gov/32084305/
- Kast JI, McFarlane AJ, Głobińska A, Sokolowska M, Wawrzyniak P, Sanak M, et al. Respiratory syncytial virus infection influences tight junction integrity. Clin Exp Immunol. 2017;190:351–9. Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5680068/
- Bikle DD. Vitamin D and the immune system: role in protection against bacterial infection. Curr Opin Nephrol Hypertens. 2008;17:348–52. Available from: https://pubmed.ncbi.nlm.nih.gov/18660668/
- Beard JA, Bearden A, Striker R. Vitamin D and the anti-viral state. J Clin Virol. 2011;50:194–200. Available from: https://pubmed.ncbi.nlm.nih.gov/21242105/
- Martineau AR, Jolliffe DA, Greenberg L, Aloia JF, Bergman P, Dubnov-Raz G, et al. Vitamin D supplementation to prevent acute respiratory infections: individual participant data meta-analysis. Health Technol Assess. 2019;23:1–44. Available from: https://pubmed.ncbi.nlm.nih.gov/30675873/
- Martineau AR, Jolliffe DA, Hooper RL, Greenberg L, Aloia JF, Bergman P, et al. Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ. 2017;356:i6583. Available from: https://www.bmj.com/content/356/bmj.i6583
- Brenner H, Holleczek B, Schöttker B. Vitamin D Insufficiency and Deficiency and Mortality from Respiratory Diseases in a Cohort of Older Adults: Potential for Limiting the Death Toll during and beyond the COVID-19 Pandemic? Nutrients [Internet]. 2020;12. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7468980/
- Grant WB, Lahore H, McDonnell SL, Baggerly CA, French CB, Aliano JL, et al. Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths. Nutrients [Internet]. 2020;12. Available from: https://pubmed.ncbi.nlm.nih.gov/32252338/
- Annweiler C, Cao Z, Sabatier J-M. Point of view: Should COVID-19 patients be supplemented with vitamin D? Maturitas. 2020;140:24–6. Available from:https://pubmed.ncbi.nlm.nih.gov/32972631/
- Hernández JL, Nan D, Fernandez-Ayala M, García-Unzueta M, Hernández-Hernández MA, López-Hoyos M, et al. Vitamin D Status in Hospitalized Patients with SARS-CoV-2 Infection. J Clin Endocrinol Metab [Internet]. 2020; Available from: https://pubmed.ncbi.nlm.nih.gov/33159440/
- Macaya F, Espejo Paeres C, Valls A, Fernández-Ortiz A, González Del Castillo J, Martín-Sánchez FJ, et al. Interaction between age and vitamin D deficiency in severe COVID-19 infection. Nutr Hosp. 2020;37:1039–42. Available from: https://pubmed.ncbi.nlm.nih.gov/32960622/
- Radujkovic A, Hippchen T, Tiwari-Heckler S, Dreher S, Boxberger M, Merle U. Vitamin D Deficiency and Outcome of COVID-19 Patients. Nutrients [Internet]. 2020;12. Available from: https://pubmed.ncbi.nlm.nih.gov/32927735/
- Baktash V, Hosack T, Patel N, Shah S, Kandiah P, Van Den Abbeele K, et al. Vitamin D status and outcomes for hospitalised older patients with COVID-19. Postgrad Med J [Internet]. 2020; Available from: https://pmj.bmj.com/content/early/2021/01/23/postgradmedj-2020-138712
- Merzon E, Tworowski D, Gorohovski A, Vinker S, Golan Cohen A, Green I, et al. Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study. FEBS J [Internet]. 2020; Available from: https://pubmed.ncbi.nlm.nih.gov/32700398/
- Jain A, Chaurasia R, Sengar NS, Singh M, Mahor S, Narain S. Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers. Sci Rep. Nature Publishing Group; 2020;10:1–8. Available from: https://www.nature.com/articles/s41598-020-77093-z
- Entrenas Castillo M, Entrenas Costa LM, Vaquero Barrios JM, Alcalá Díaz JF, López Miranda J, Bouillon R, et al. “Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study.” J Steroid Biochem Mol Biol. 2020;203:105751. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7456194/
- Li G, Fan Y, Lai Y, Han T, Li Z, Zhou P, et al. Coronavirus infections and immune responses. J Med Virol. 2020;92:424–32. Available from: https://pubmed.ncbi.nlm.nih.gov/31981224/
- Yao XH, Li TY, He ZC, Ping YF, Liu HW, Yu SC, et al. [A pathological report of three COVID-19 cases by minimal invasive autopsies]. Zhonghua Bing Li Xue Za Zhi. 2020;49:411–7. Available from: https://pubmed.ncbi.nlm.nih.gov/32172546/
- Daneshkhah A, Agrawal V, Eshein A, Subramanian H, Roy HK, Backman V. The possible role of Vitamin D in suppressing cytokine storm and associated mortality in COVID-19 patients. MedRxiv. Cold Spring Harbor Laboratory Press; 2020; Available from: https://www.medrxiv.org/content/10.1101/2020.04.08.20058578v4
- Tan Z-X, Chen Y-H, Xu S, Qin H-Y, Zhang C, Zhao H, et al. Calcitriol inhibits bleomycin-induced early pulmonary inflammatory response and epithelial-mesenchymal transition in mice. Toxicol Lett. 2016;240:161–71. Available from: https://pubmed.ncbi.nlm.nih.gov/26520185/
- Takano Y, Mitsuhashi H, Ueno K. 1α,25-Dihydroxyvitamin D₃inhibits neutrophil recruitment in hamster model of acute lung injury. Steroids. 2011;76:1305–9. Available from: https://pubmed.ncbi.nlm.nih.gov/21745487/
- Kaufman HW, Niles JK, Kroll MH, Bi C, Holick MF. SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels. PLoS One. 2020;15:e0239252. Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0239252
- D’Avolio A, Avataneo V, Manca A, Cusato J, De Nicolò A, Lucchini R, et al. 25-Hydroxyvitamin D Concentrations Are Lower in Patients with Positive PCR for SARS-CoV-2. Nutrients [Internet]. 2020;12. Available from: https://pubmed.ncbi.nlm.nih.gov/32397511/
- Meltzer DO, Best TJ, Zhang H, Vokes T, Arora V, Solway J. Association of Vitamin D Status and Other Clinical Characteristics With COVID-19 Test Results. JAMA Netw Open. 2020;3:e2019722. Available from:https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2770157
- Alipio M. Do Latitude and Ozone Concentration Predict COVID-2019 Cases in 34 Countries? [Internet]. 2020 [cited 2020 Jul 16]. Available from: https://www.medrxiv.org/content/10.1101/2020.04.09.20060202v1




